
By Cynthia Boyd, MD, MPH
Associate Professor, Johns Hopkins Bloomberg School of Public Health
Introduction
While the prevalence of having multiple chronic conditions, or multimorbidity, increases with age, the numbers of people living with multimorbidity of all ages is increasing.1 Forty-eight percent of older adults have 3 or more chronic conditions.2 Many people living with multiple chronic conditions are less than 60 years of age. 3,4 In younger populations, 35 percent of disabled adults have 3 or more chronic conditions.5 Among children, where the definition of a chronic condition is less clear, prevalence estimates range from less than 1 percent up to 44 percent of children living with multiple chronic conditions.6 The presence of multiple chronic conditions is especially important when each condition may influence the care of the other condition(s) through limitations of life expectancy, interactions between drug therapies, and/or direct contraindications to therapy for one condition by other conditions.7-10
The Role of Guidelines:
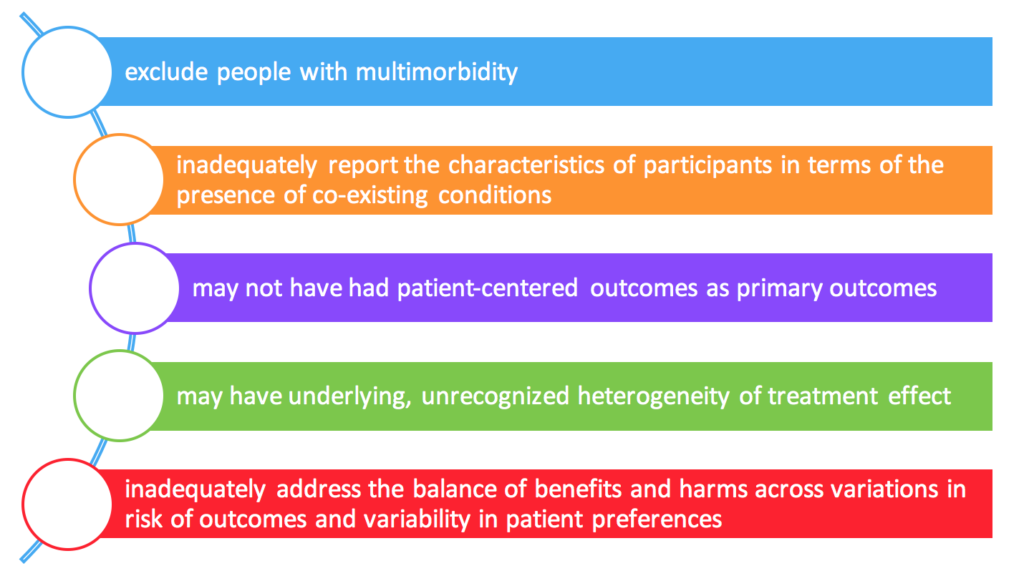
Our existing evidence base often struggles to adequately inform patient-centered care for people with multiple chronic conditions, or multimorbidity.11 Guidelines focused on specific individual conditions may not be applicable to people with multiple chronic conditions.11-14 Primary studies often:
We can’t forget though, that as the Institute of Medicine noted,
“Clinical practice guidelines are statements that include recommendations intended to optimize patient care that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options. Rather than dictating a one-size-fits-all approach to patient care, clinical practice guidelines offer an evaluation of the quality of the relevant literature and an assessment of the likely benefits and harms of a particular treatment. This information enables providers to proceed accordingly, selecting the best care for a unique patient based on his or her preferences.”15
This definition, and goal, is exactly what is needed for people with multiple chronic conditions. Despite this ideal, developing guidelines that inform person-centered care for people with multiple chronic conditions is challenging, and the relevance of these guidelines is limited.11-14
What's New?
These are exciting times for the realm of multimorbidity in guidelines. Efforts to address this growing population are underway around the world. There is not a universal answer on how best to address people with multiple chronic conditions in guidelines; rather it depends on the specific question being addressed.
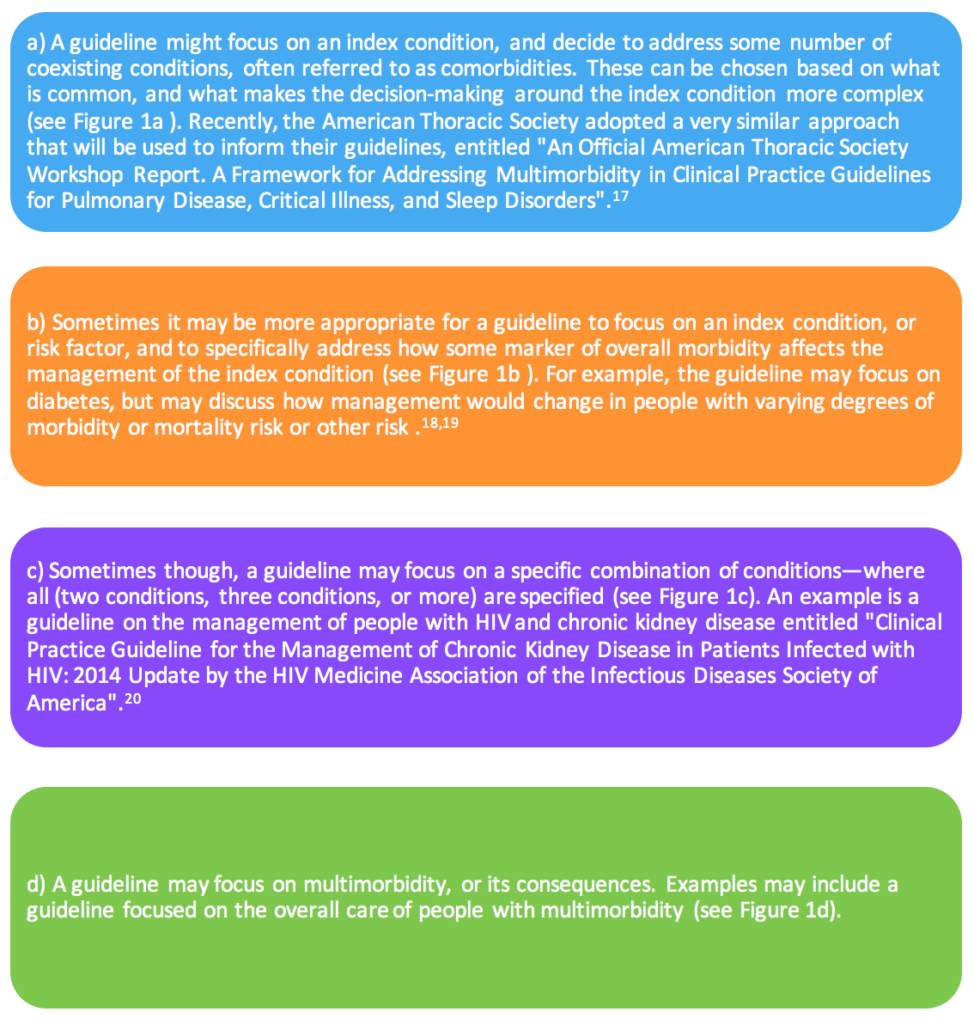
How might guidelines increase their relevance to the care of people living with multiple chronic conditions? A stakeholder informed framework was developed that illustrates several key frames that can be used to inform trustworthy guidelines:16
The National Institute for Health and Care Excellence in the United Kingdom recently published a guideline on Multimorbidity: Clinical Assessment and Management. The NICE guideline covers optimizing care for adults with multimorbidity through several key recommendations:
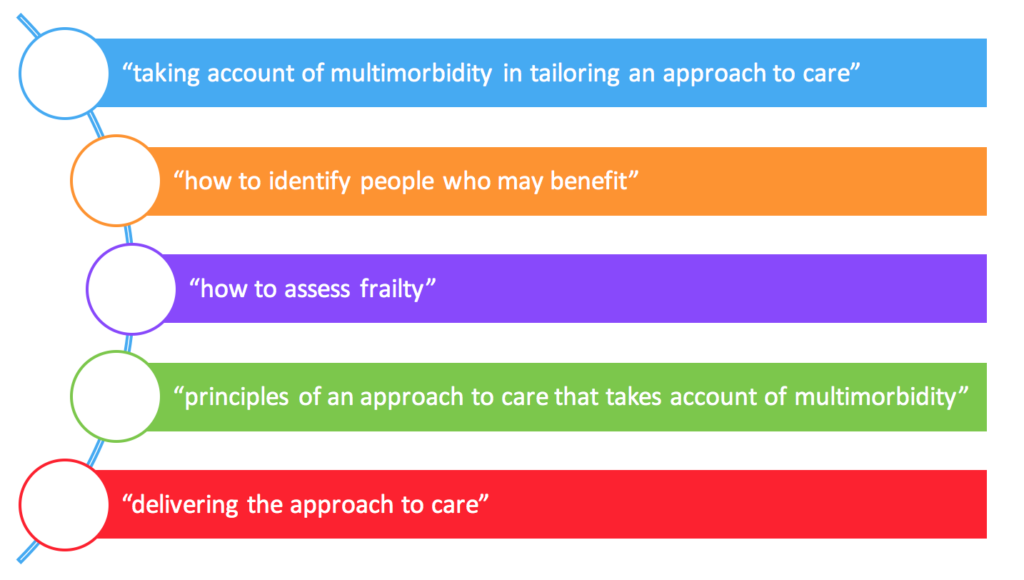
The guideline addresses several key issues that matter to people with multiple chronic conditions, including reducing treatment burden (polypharmacy and multiple appointments). Second, the approach to care recommended for this population specifically focuses on shared decision making based on what is important to the person.
What’s Next:
This is just a snippet of all the innovative work being done to address the exciting opportunity to meet the needs of people living with multimorbidity through evidence-based medicine and person-centered care. These concepts are in no way contradictory to each other – our challenge, and work ahead, is to make sure both are realities for people living with multimorbidity.
References:
- Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. 2008;14 Suppl 1:28-32.
- Anderson G, Horvath J. Chronic Conditions: Making the Case for Ongoing Care. Partnership for Solutions; 2002.
- Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2005;3(3):223-228.
- Fortin M, Hudon C, Haggerty J, Akker M, Almirall J. Prevalence estimates of multimorbidity: a comparative study of two sources. BMC Health Serv Res. 2010;10:111.
- Kronick RG, Bella M, Gilmer TP, Somers SA. The faces of Medicaid II: Recognizing the care needs of people with multiple chronic conditions. Center for Health Care Strategies, Inc.; October 2007.
- van der Lee JH, Mokkink LB, Grootenhuis MA, Heymans HS, Offringa M. Definitions and measurement of chronic health conditions in childhood: a systematic review. JAMA. 2007;297(24):2741-2751.
- AHRQ. Optimizing prevention and healthcare management for the complex patient (R21). 2007.
- Safford MM, Allison JJ, Kiefe CI. Patient complexity: more than comorbidity. the vector model of complexity. J Gen Intern Med. 2007;22 Suppl 3:382-390.
- Parekh AK, Barton MB. The challenge of multiple comorbidity for the US health care system. JAMA. 2010;303(13):1303-1304.
- Parekh AK, Goodman RA, Gordon C, Koh HK. Managing multiple chronic conditions: a strategic framework for improving health outcomes and quality of life. Public Health Rep. 2011;126(4):460-471.
- Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716-724.
- Fortin M, Contant E, Savard C, Hudon C, Poitras ME, Almirall J. Canadian guidelines for clinical practice: an analysis of their quality and relevance to the care of adults with comorbidity. BMC Fam Pract. 2011;12:74.
- Lugtenberg M, Burgers JS, Clancy C, Westert GP, Schneider EC. Current Guidelines Have Limited Applicability to Patients with Comorbid Conditions: A Systematic Analysis of Evidence-Based Guidelines. PLoS ONE 2011;6(10):e25987.
- Mutasingwa DR, Ge H, Upshur RE. How applicable are clinical practice guidelines to elderly patients with comorbidities? Can Fam Physician. 2011;57(7):e253-262.
- Guidelines CoSfDTCP, Medicine Io. Clinical Practice Guidelines We Can Trust. The National Academies Press; 2011.
- Uhlig K, Leff B, Kent D, et al. A framework for crafting clinical practice guidelines that are relevant to the care and management of people with multimorbidity. J Gen Intern Med. 2014;29(4):670-679.
- Wilson KC, Gould MK, Krishnan JA, et al. An Official American Thoracic Society Workshop Report. A Framework for Addressing Multimorbidity in Clinical Practice Guidelines for Pulmonary Disease, Critical Illness, and Sleep Disorders. Ann Am Thorac Soc. 2016;13(3):S12-21.
- You JJ, Singer DE, Howard PA, et al. Antithrombotic Therapy for Atrial Fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2_suppl):e531S-e575S.
- Mangione CM, Moreno G, Geffen D, et al. Guidelines abstracted from the American Geriatrics Society Guidelines for Improving the Care of Older Adults with Diabetes Mellitus: 2013 update. J Am Geriatr Soc. 2013;61(11):2020-2026.
- Lucas GM, Ross MJ, Stock PG, et al. Clinical practice guideline for the management of chronic kidney disease in patients infected with HIV: 2014 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(9):e96-138.
About the author:
Dr. Cynthia Boyd, MD MPH is an Associate Professor of Medicine in the Division of Geriatric Medicine and Gerontology at Johns Hopkins University School of Medicine. She has focused her research career on the care of people with multiple chronic conditions, including the development and application of guidelines for people living with multiple chronic conditions, or multimorbidity.
Dr. Boyd led an Agency for Health Care Research and Quality (AHRQ) funded project to develop recommendations for how to make the translational path from evidence generation to evidence synthesis to guideline development more relevant to people with multiple chronic conditions. In collaboration with partners from Kaiser Permanente’s National Guideline Program, she is currently leading a PCORI-funded project entitled "Informing Patient-Centered Care of People with Multiple Chronic Conditions.”